Humanism in Medical Education
If someone says “humanism in medicine,” what does that mean to you? How do we define a humanistic physician? Many will consider qualities that emphasize connection between the physician and their patient, but it may be more challenging to consider how these qualities can be developed or taught.
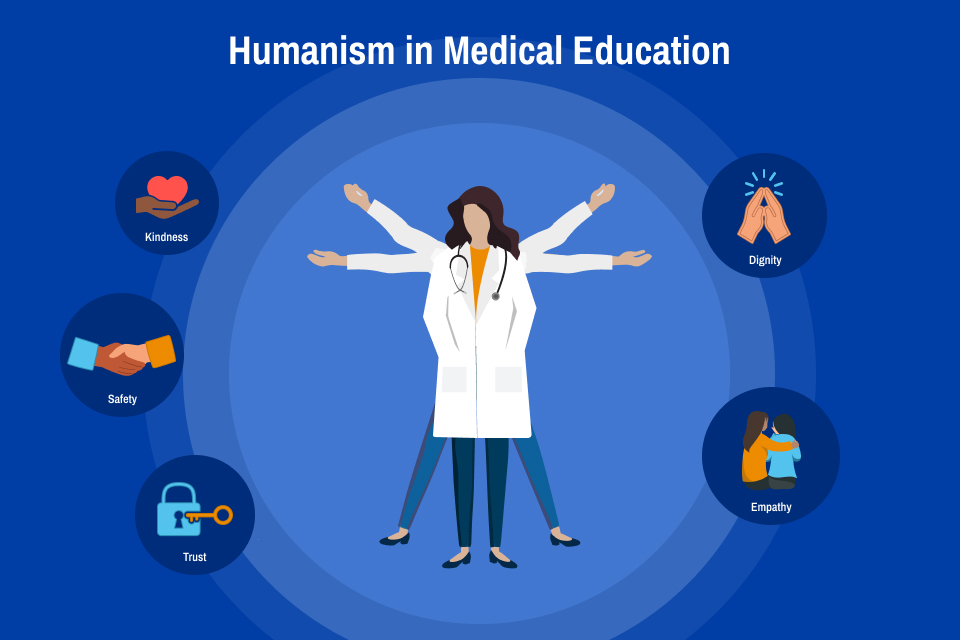
Both the LCME and the ACGME, major accreditation councils for undergraduate and graduate medical education, value humanism. The LCME requires that all medical schools include material on medical ethics and human values, with a recent review exploring how this is implemented and the impacts of such curricula. The ACGME incorporates humanistic ideals into its professionalism competency, with a priority to demonstrate “compassion, integrity and respect for others.” Humanism in medicine can be described as maintaining a focus on the human dignity of each patient, recognizing the importance of understanding unique, individualized needs of each patient and viewing patients from a wholistic and understanding lens. In medicine, it is essential to maintain this humanistic approach and encourage these traits in our colleagues. Since 1988, the Gold Foundation has been dedicated to promoting humanism in medicine, offering education, community building, and recognition for physicians and trainees who demonstrate humanistic qualities—described by the organization as care established in kindness, safety and trust. Means to enhance humanism in medicine include promoting values that center on patient dignity, recognition of the humanity of all patients, and empathetic connection with others.
By fostering humanism in medicine, we can impact our patients’ health outcomes. Empathy - the ability to relate on a deep human level to another - is a key component of medical humanism. The connection between a provider’s empathy and their patient’s outcomes has been demonstrated repeatedly. Patients who rate their physicians higher in empathy have better outcomes in a wide variety of conditions—diabetes mellitus, psychiatric disorders, and even quality of life scores in oncology. By empowering physicians and trainees to connect more deeply with their patients’ humanity, we often see improved patient care and end results. Cultivating humanism can be an effective way to enhance patient trust, leading to improved adherence to lifestyle modifications or treatment plans.
Humanism benefits more than just our patients. Physicians who have a higher empathetic connection to their patients and who appreciate more personal meaning in their work have lower rates of burnout and depression. This is especially critical in the post-pandemic landscape, where burnout among health care providers is rising. One proposed solution to the damaging “health care hero” mentality on the well-being of providers is to lean back into the “humanism” approach—fostering deeper connection in the attempt to benefit both patients and medical providers.
Knowing that humanistic physicians can benefit all, how do medical educators best cultivate these skills in trainees? If humanism focuses on connection and centering human communication, how do we best develop expertise? At an individual level, humanism can be practiced by promoting patient-first language or learning non-medical information about each patient. Providers should practice active listening and allow patients to express their own priorities in each encounter. Body language cues such as sitting down and maintaining open posture can be small ways to encourage human connection. Pausing to recognize intrinsic biases or challenging stereotypes is another way to promote humanism in our daily work. Instructors can consider encouraging students to learn about their patients’ past, family members, or hobbies outside of the traditional medical visit script.
Current efforts are underway at Cardinal Glennon Children’s Hospital to determine the impact of a humanism-focused curriculum on resident well-being. We plan to include individual content such as guided meditation, mindfulness practice, prompted journaling, art and music to enhance self-awareness and foster connection. The new curriculum also emphasizes connection with community advocates, specifically through lenses of diversity and inclusion, as well as discussion about the intersection between pediatric health issues and social determinants of health. Our hope is that by encouraging residents to take time in their busy schedules to deeply connect with themselves and their community, we will see reduced burnout in residents and improved patient satisfaction with provider connection.
Infusing medical humanism curricula throughout the medical education training spectrum can benefit our individual wellness, the clinical learning environment, and the patients we serve. Opportunities to include this essential component in structured curricula should be intentionally sought and implemented by educators.
More resources for teaching humanities in medicine have emerged in the last several years, including “Twelve tips on teaching and learning humanism in medical education,” which provides a framework for medical educators that can be applied across many settings. A more recent study explores the importance of humanism education during residency; residents agree that these skills are important to continue to cultivate in graduate medical education.

Kayla Heller, M.D., is an associate professor of pediatrics and program director of the Pediatric Residency Program at Saint Louis University SSM Health Cardinal Glennon Children’s Hospital. Heller completed a Master of Health Professions Education at the University of Missouri School of Medicine. Heller's areas of professional interest include simulation, curriculum development, and program evaluation. Heller can be contacted via email.